MRSA Infection: What You Need to Know\n\n## What Exactly is MRSA? Understanding the Basics\n\nHey guys, ever heard of
MRSA
? This super bug, short for
Methicillin-resistant Staphylococcus aureus
, is a type of staph bacteria that’s become a real headache because it’s resistant to several common antibiotics. Now, don’t get it twisted –
Staphylococcus aureus
or “staph” is actually a pretty common bacterium. Many of us, about one in three people, actually carry staph on our skin or in our noses without ever getting sick. It’s usually harmless when it stays on the surface of your skin. But here’s the kicker: when staph gets into the body through a cut, scrape, or wound, it can cause infections. And
that’s
when things can get serious, especially if it’s the
MRSA
strain. Think of it like this: regular staph is like a common cold, annoying but usually manageable.
MRSA
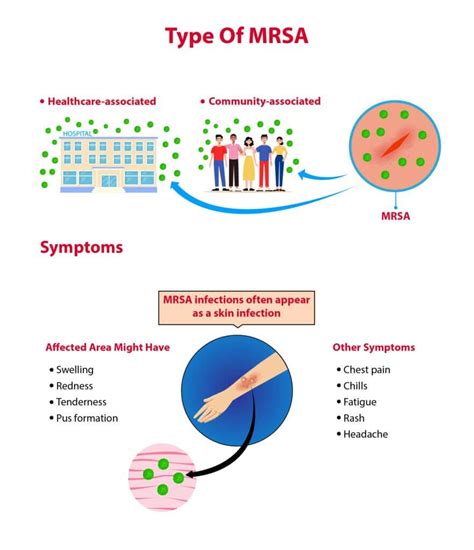
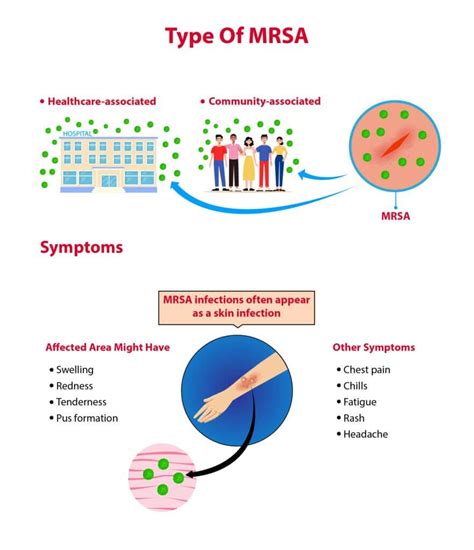
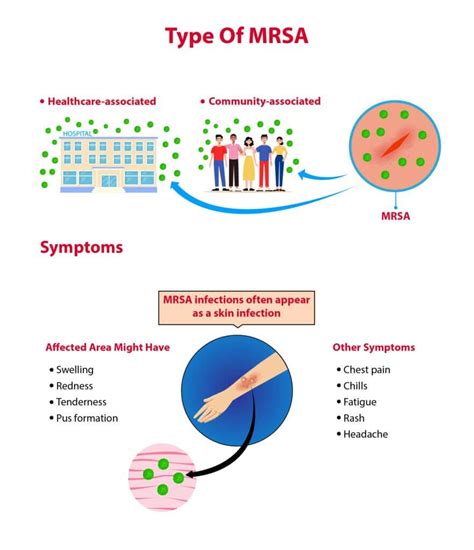
, however, is like a super-cold that laughs in the face of your usual remedies. This resistance is why MRSA is such a concern; it makes treating infections much more challenging and can lead to more severe outcomes. The “methicillin-resistant” part of its name specifically means it’s impervious to methicillin and other related antibiotics, like oxacillin, penicillin, and amoxicillin. This significantly limits the drug options available for effective treatment, often requiring stronger or more specialized antibiotics, which might also have more side effects. It’s not just a hospital bug anymore, either. While
MRSA
used to be primarily associated with healthcare settings (often called HA-MRSA), we’ve seen a significant rise in
community-associated MRSA
(CA-MRSA) infections. These are infections that develop in people who haven’t had recent contact with healthcare facilities, like hospitals or nursing homes. This means it can spread in places like gyms, schools, locker rooms, or even at home. Understanding what MRSA is, how it differs from regular staph, and why its resistance is a big deal is the very first step in protecting yourself and those around you from this increasingly common and potentially serious infection. It’s truly a global health challenge, and awareness is our first line of defense.\n\n## How Does MRSA Spread? Common Transmission Routes\n\nSo, how exactly does this pesky
MRSA
get around, you ask? Well, it’s pretty good at spreading, primarily through
direct skin-to-skin contact
with an infected person or by touching objects contaminated with the bacteria. Imagine this scenario: someone with an
MRSA
skin infection touches a surface like a doorknob, a shared razor, or even gym equipment. The bacteria can then hang out on that surface, just waiting for the next person to come along and touch it. If that person then touches their own skin, especially an open wound or a break in the skin, boom –
MRSA
has found a new home. This is why proper hygiene is so incredibly crucial, guys. In healthcare settings, it’s often spread through the hands of healthcare workers who might not have thoroughly washed or sanitized their hands between patients. This is the classic route for
Hospital-Associated MRSA
(HA-MRSA). Think about the high-touch surfaces in a hospital room – bed rails, IV poles, call buttons – these can all become transmission points if not meticulously cleaned. But as we discussed,
Community-Associated MRSA
(CA-MRSA) is also a major concern. This strain is often found in places where people are in close contact or share items. Think of athletes in locker rooms sharing towels or equipment, or even kids at school.
MRSA
can also be transmitted through sharing personal items like razors, towels, clothing, or even sports gear that hasn’t been properly cleaned. It loves warm, moist environments, which is why things like shared damp towels are a big no-no. It’s important to remember that
MRSA
doesn’t typically spread through the air, like a cold or flu virus. You generally won’t catch it just by being in the same room as someone who has it, unless you have direct contact with their infected skin or contaminated objects. However, someone carrying
MRSA
in their nose or throat can potentially spread it through respiratory droplets, though this is less common than direct skin contact. The key takeaway here is that
MRSA
is a contact sport – it needs a direct or indirect touch to spread. Understanding these common transmission routes empowers us to take proactive steps to break the chain of infection and protect ourselves and our loved ones.\n\n## Recognizing the Signs: What Does an MRSA Infection Look Like?\n\nAlright, let’s talk about what to look for, because recognizing the signs of an
MRSA
infection early can make a huge difference in treatment and preventing more serious issues. Most
MRSA
infections actually start out as skin infections, and they can often be mistaken for something else at first – maybe a spider bite, a pimple, or a boil. But here’s the crucial part, guys: an
MRSA
skin infection usually appears as a red, swollen, painful bump that might feel warm to the touch. It often looks like a
pustule
or a
boil
, and sometimes it has a head and can be full of pus or other drainage. You might also notice a fever alongside these symptoms, which is your body’s way of fighting off infection. The area around the bump might also be inflamed and tender. Unlike a typical pimple that might go away on its own,
MRSA
infections often get worse and can be quite persistent. The infection can grow larger, become more painful, and might even develop into an abscess that requires drainage. If not treated, these skin infections can spread further into the skin and soft tissues, leading to a condition called
cellulitis
, which is a deeper and more widespread infection characterized by redness, swelling, and warmth that spreads rapidly. But wait, it can get even more serious. While skin infections are the most common,
MRSA
can also cause more severe types of infections if it gets into the bloodstream, lungs, bones, or other organs. For example, it can lead to pneumonia (a serious lung infection), bloodstream infections (sepsis), bone infections (osteomyelitis), or even infections of the heart valves (endocarditis). These internal infections are much more dangerous and can be life-threatening, requiring intensive medical care. Symptoms for these more severe infections would depend on the site of infection but could include persistent fever, chills, shortness of breath, chest pain, severe body aches, or a general feeling of being very unwell. The key message here is: if you have a skin lesion that is red, swollen, painful, warm, or draining pus, and it’s not improving or seems to be getting worse,
especially
if you also have a fever, don’t just brush it off as a harmless bug bite. Get it checked out by a healthcare professional immediately. Early diagnosis and treatment are absolutely vital to prevent
MRSA
from causing more extensive damage and becoming a much bigger problem.\n\n## Who is at Risk? Identifying Vulnerable Populations\n\nLet’s talk about who needs to be extra vigilant when it comes to
MRSA
, because while anyone can get infected, certain groups are definitely more susceptible. Understanding these risk factors can help you take proactive steps to protect yourself and your loved ones. First up, we have individuals in
healthcare settings
. This includes patients in hospitals, nursing homes, and other long-term care facilities, as well as healthcare workers themselves. The reason is pretty straightforward: these environments often have a higher concentration of
MRSA
bacteria, and people there are often more vulnerable due to weakened immune systems, open wounds from surgery, or indwelling medical devices like catheters or IV lines. Healthcare workers are at risk because they have frequent contact with patients who might be colonized or infected with
MRSA
. Next, people who have had
recent surgery or other invasive medical procedures
are also at heightened risk. Any break in the skin, whether from a surgical incision, a wound, or an IV insertion site, creates an entry point for bacteria like
MRSA
to get into the body and cause an infection. Similarly, individuals with
weakened immune systems
, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, organ transplant recipients on immunosuppressant drugs, or people with chronic illnesses like diabetes or kidney disease, are more vulnerable. Their bodies simply aren’t as equipped to fight off infections. But it’s not just about hospitals, guys!
Community-associated MRSA
(CA-MRSA) has its own set of risk factors. This includes
athletes
who participate in contact sports or share equipment in locker rooms. Skin-to-skin contact, minor cuts and abrasions that occur during sports, and shared items like towels or protective gear can all contribute to
MRSA
spread. Places that are
crowded, such as dormitories, military barracks, or even prisons
, can also be hotbeds for
MRSA
transmission due to close living quarters and shared facilities. People who
inject drugs
are also at a significantly higher risk due to skin punctures and potentially unsterile injection practices. Even having
open wounds, cuts, or abrasions
that aren’t properly covered can put anyone at higher risk, regardless of their other health status. And finally, repeated or
inappropriate antibiotic use
can contribute to the development of resistant bacteria like
MRSA
. While antibiotics are crucial for fighting bacterial infections, using them when they’re not needed (like for viral infections) or not completing a full course can inadvertently promote resistance. So, if you fall into any of these categories or know someone who does, it’s even more important to be aware of
MRSA
and practice excellent hygiene and preventive measures. Stay safe and informed, everyone!\n\n## Diagnosis and Treatment: Battling MRSA Effectively\n\nAlright, so you suspect you or someone you know might have
MRSA
. What happens next? The good news is that
MRSA
can
be treated, but it requires proper diagnosis and often specific antibiotics. The first step in battling
MRSA
effectively is accurate diagnosis. If you visit your doctor with symptoms suggestive of a skin infection, they’ll likely take a
swab sample
from the infected area – for instance, from a skin lesion, a wound, or even from your nose if they suspect you’re a carrier. This sample is then sent to a lab for a
bacterial culture
. The lab will grow the bacteria and then test it to see which antibiotics it’s resistant to. This is called
antibiotic susceptibility testing
, and it’s absolutely crucial for confirming if it’s
MRSA
and determining the most effective treatment. Sometimes, if the infection is deeper or more serious (like pneumonia or a bloodstream infection), blood, urine, or tissue samples might be taken instead. Once
MRSA
is confirmed, your doctor will determine the best course of action. For localized skin infections like boils or abscesses, the primary treatment often involves
draining the pus
. This can sometimes be done in the doctor’s office and is a very effective way to remove the source of the infection. Your doctor might also prescribe antibiotics. Now, because
MRSA
is resistant to many common antibiotics, they’ll need to choose specific ones that are known to be effective against it. These might include antibiotics like clindamycin, trimethoprim-sulfamethoxazole (Bactrim), doxycycline, or linezolid. For more severe or widespread infections, intravenous (IV) antibiotics might be necessary, often requiring hospitalization. Here’s a super important point, guys: if you’re prescribed antibiotics, you
must
complete the entire course
, even if you start feeling better after a few days. Stopping early can lead to the infection coming back stronger and potentially contributing to further antibiotic resistance. It’s also vital to follow all wound care instructions carefully, keeping the area clean and covered to prevent further spread. Your doctor might also recommend decolonization strategies for recurrent
MRSA
carriers, which can involve antiseptic washes or nasal ointments. Don’t try to self-diagnose or treat
MRSA
with over-the-counter remedies. It’s a serious infection that requires professional medical attention. The key to successful treatment is timely diagnosis, appropriate antibiotic selection based on susceptibility testing, and strict adherence to the treatment plan. Stay diligent and work closely with your healthcare provider to kick
MRSA
to the curb!\n\n## Prevention is Key: Simple Steps to Protect Yourself\n\nAlright, now for one of the most important sections, guys: how to
prevent
getting or spreading
MRSA
! Because when it comes to any infection, prevention is always better than cure, especially with a tricky bug like
MRSA
. The good news is that many prevention strategies are simple, everyday habits that we should all be practicing anyway. First and foremost, let’s talk about the absolute champion of infection prevention:
hand hygiene
. Wash your hands frequently and thoroughly with soap and water for at least 20 seconds, especially after using the restroom, before eating, after coughing or sneezing, and after touching shared surfaces. If soap and water aren’t available, use an alcohol-based hand sanitizer with at least 60% alcohol. This simple act is incredibly effective at removing
MRSA
and many other germs. Next up,
proper wound care
is crucial. If you have any cuts, scrapes, or open wounds, keep them clean and covered with a sterile, dry bandage. This not only protects the wound from infection but also prevents any
MRSA
you might be carrying from spreading to others. Change bandages as directed by your doctor, or when they become wet or dirty. Seriously, don’t leave wounds exposed and vulnerable. Another big one:
avoid sharing personal items
. This means no sharing razors, towels, washcloths, clothing, uniforms, or even athletic equipment that comes into direct skin contact.
MRSA
loves to hitch a ride on these items, especially if they’re damp. Each person should have their own personal care items, and these should be cleaned regularly. For athletes, it’s essential to shower immediately after practices and games, using soap, and to wash athletic gear after each use. Regular cleaning and disinfection of frequently touched surfaces in your home, workplace, and gym can also make a big difference. Use a household cleaner or disinfectant to wipe down doorknobs, light switches, countertops, and shared equipment. When you’re in healthcare settings, don’t hesitate to remind healthcare providers to wash their hands or use hand sanitizer before and after touching you. It’s your right to ask! And finally, let’s touch on
responsible antibiotic use
. Don’t pressure your doctor for antibiotics if they say you don’t need them (e.g., for a cold or flu, which are viral infections). If you are prescribed antibiotics, take them exactly as directed and complete the entire course. This helps prevent the development of antibiotic-resistant bacteria like
MRSA
. By consistently practicing these simple yet powerful prevention steps, you can significantly reduce your risk of
MRSA
infection and contribute to a healthier community for everyone. It’s all about being smart and proactive, guys!\n\n## Living with MRSA: Managing and Preventing Recurrence\n\nSo, you’ve had
MRSA
– now what? Living with a history of
MRSA
means understanding how to manage it and, even more importantly, how to prevent it from coming back or spreading to others. It’s totally doable, but it requires ongoing diligence and awareness. First and foremost, if you’ve been diagnosed with
MRSA
, it’s essential to
inform your healthcare providers
during every visit, including doctors, nurses, and even dentists. This allows them to take appropriate precautions, like using contact isolation, to prevent
MRSA
spread to other patients and to ensure they select effective treatments if you develop another infection. It also helps them tailor any future medical care to your specific needs, knowing your history with a resistant bacterium. Continuing with
excellent personal hygiene
is non-negotiable. This means maintaining strict handwashing habits, even when you’re feeling perfectly healthy. Wash your hands frequently with soap and water, especially after touching your skin, going to the bathroom, or before preparing food. If recommended by your doctor, you might need to use special antiseptic soaps or nasal ointments as part of a decolonization regimen, especially if you’re a carrier or have had recurrent infections. Always follow these instructions carefully.
Meticulous wound care
is also paramount. Any cuts, scrapes, or wounds must be kept clean and covered with fresh, dry bandages until they are completely healed. Avoid picking at scabs or draining any lesions yourself, as this can worsen the infection and increase the risk of spread. If you notice any new skin lesions, especially those that are red, swollen, painful, or draining, seek medical attention promptly. Early intervention is key to preventing a minor issue from escalating. Furthermore, continue to
avoid sharing personal items
like towels, razors, or athletic gear. Ensure these items are regularly cleaned or, where appropriate, disposed of after use. Washing laundry, especially items that have come into contact with skin or wounds, in hot water with detergent can help eliminate
MRSA
bacteria. Regular cleaning and disinfecting of surfaces in your home that are frequently touched is also a good practice. Understand that being colonized with
MRSA
(meaning you carry the bacteria without having an active infection) is common, and you might always carry it. The goal is to prevent it from causing an active infection. By consistently adhering to these practices, you not only protect yourself from recurrence but also play a vital role in preventing the spread of
MRSA
within your family and community. It’s about taking charge of your health and being a responsible member of the broader community, guys!